Key Takeaways
- About 33% of nurses report high emotional exhaustion.
- Burnout prevalence: US 28.3%, Europe 15.8%, Asia 22.7%, Africa 52.9%.
- COVID-focused units recorded 39.23% high exhaustion.
- 57% report feeling exhausted every day.
- 60% cite unresponsive leadership as a driver.
- 29% of LPNs/LVNs report mandated overtime.
- 23% of U.S. nurses are considering leaving.
- A 10% rise in exit intent aligns with 14% higher mortality.
- Replacing one RN costs roughly $50k to $73k.
Nurse burnout is a form of occupational exhaustion. Signs and symptoms of nurse burnout include emotional fatigue, depersonalisation, and a reduced sense of personal accomplishment. Around one-third of nurses worldwide report high emotional exhaustion, with prevalence ranging from roughly one-quarter of the nursing workforce in some regions to more than half in others.
If you’re a nursing student, you might want to work with an essay writer without AI. EssayHub can help you explore this topic, offering nursing burnout statistics in depth while supporting you in managing your own workload.
General Nurse Burnout Statistics
A quick pulse check helps frame the problem. Here’s the big picture showing nursing burnout rates, kept simple and useful.
- Overall prevalence. About one-third of nurses report high emotional exhaustion. Around one quarter report high depersonalization, and roughly one third report low personal accomplishment.
- Regional differences. Estimated burnout prevalence clusters near 28.3% in the United States, 15.8% in Europe, 22.7% in Asia, and about 52.9% in Africa.
- Post-COVID shifts. High-acuity areas stayed elevated after the COVID-19 pandemic. Recent snapshots show emergency and ICU nurses with 35.4% overall burnout, with about 39% reporting high emotional exhaustion on COVID-focused units, and daily exhaustion self-reports around 57%.
- Workplace experience. Daily fatigue remains high, with 57% of nurses saying they feel worn out every day.
- Leadership and workload strain. 60% of nurses cite unresponsive leadership as a key driver of burnout, while 29% of LPNs and LVNs report mandated overtime that compounds schedule stress.
- Turnover intention. In the U.S., approximately 23% of nurses are considering leaving the profession, which is closely linked to issues such as workload, leadership gaps, and emotional exhaustion.
Nurse Burnout Symptoms
Burnout rarely shows up as a single sign: emotional drain pairs with small cognitive slips, and physical strain accompanies moral distress. When two or more arrive together, risk rises fast.
Signs of nurse burnout include:
- Emotional exhaustion
- Detachment and irritability
- Diminished personal accomplishment
- Cognitive overload
- Physical strain
- Moral distress
- Withdrawal from learning and teams
Emotional exhaustion alone hurts well-being. Pair it with cognitive overload and moral distress, and patient safety begins to wobble. Spotting the combinations early gives leaders room to adjust staffing, redistribute tasks, and open space for recovery before outcomes slide.
What Causes Nurse Burnout?
It’s mainly caused by a persistent mismatch between demand, control, and recovery. Causes of nurse burnout include high patient loads, limited autonomy, and thin recovery windows. When these stack together, burnout follows. Here’s how the main drivers fit together and why they compound.
- When decisions happen far from the point of care, work feels mechanical and meaning fades. 60% of nurses report unresponsive leadership as a key driver of burnout.
- Rotating nights, long stretches without a true day off, and last-minute changes make fatigue the default. 29% of LPNs/LVNs report mandated overtime, signaling schedule strain that accelerates burnout.
- Childcare, eldercare, and commute time collide with rigid rosters. 54% of nurses cited unequal work-life balance, which shows up as irritability on shift and rumination after shift.
Burnout Statistics by Specialty
Burnout rate for nurses varies by specialty. Clinical intensity shapes burnout risk. High-acuity settings compress time, raise cognitive load, and heighten moral distress, especially with frequent exposure to patient deaths.
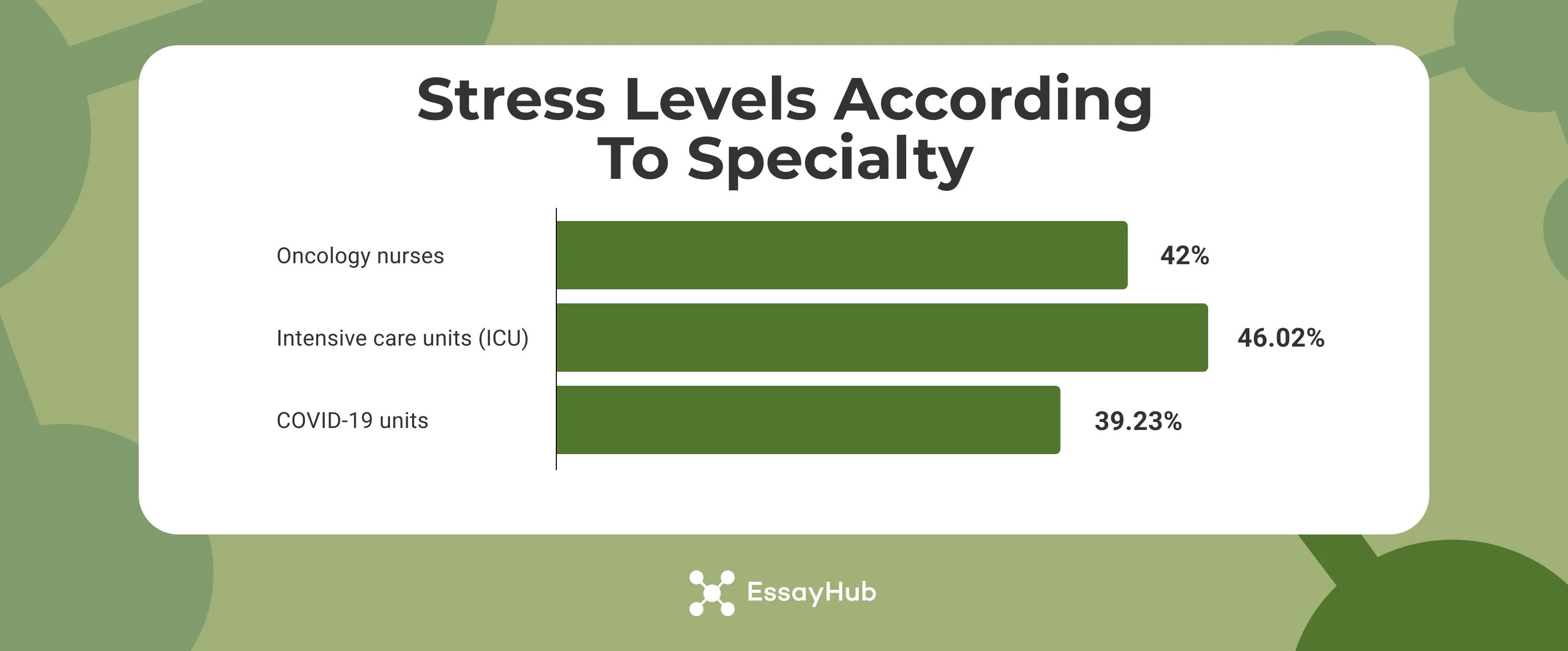
- Oncology nurses show the highest depersonalisation at 42%.
- Intensive care units show the highest low personal accomplishment at 46.02%.
- Units caring for people with COVID-19 recorded 39.23% high emotional exhaustion.
As for the license, burnout patterns shift because of daily demands, control, and recovery time.
- Registered nurses (RNs): This group reports moderate to high burnout. Common triggers include unmanageable nurse-to-patient ratios, salary dissatisfaction, and weak managerial response.
- Licensed practical/licensed vocational nurses (LPNs/LVNs): Fatigue rises with schedule pressure. Mandated overtime is common, and 29% report being required to work extra hours, which accelerates stress and exit intent.
- Advanced practice registered nurses (APRNs): Pay satisfaction runs higher, yet burnout stems from role ambiguity, administrative burden, and productivity metrics in outpatient settings.
Demographic Breakdown of Nurse Burnout
Burnout clusters around identity and context. Gender, age, and region shape how stress feels, how often it appears, and how quickly it affects patient outcomes. The patterns below point to different risks and different fixes.
Burnout Statistics by Gender
Start with the split everyone sees in the unit. Women make up most of the nursing workforce, and many report stronger salary dissatisfaction and more intimidation from colleagues. Men represent a smaller share, yet show slightly higher compassion fatigue and a higher intent to leave. In recent surveys, men reported compassion fatigue at about 48 percent and women at about 46 percent. Exit intent shows a similar gap: roughly 28 percent for men and 22 percent for women.
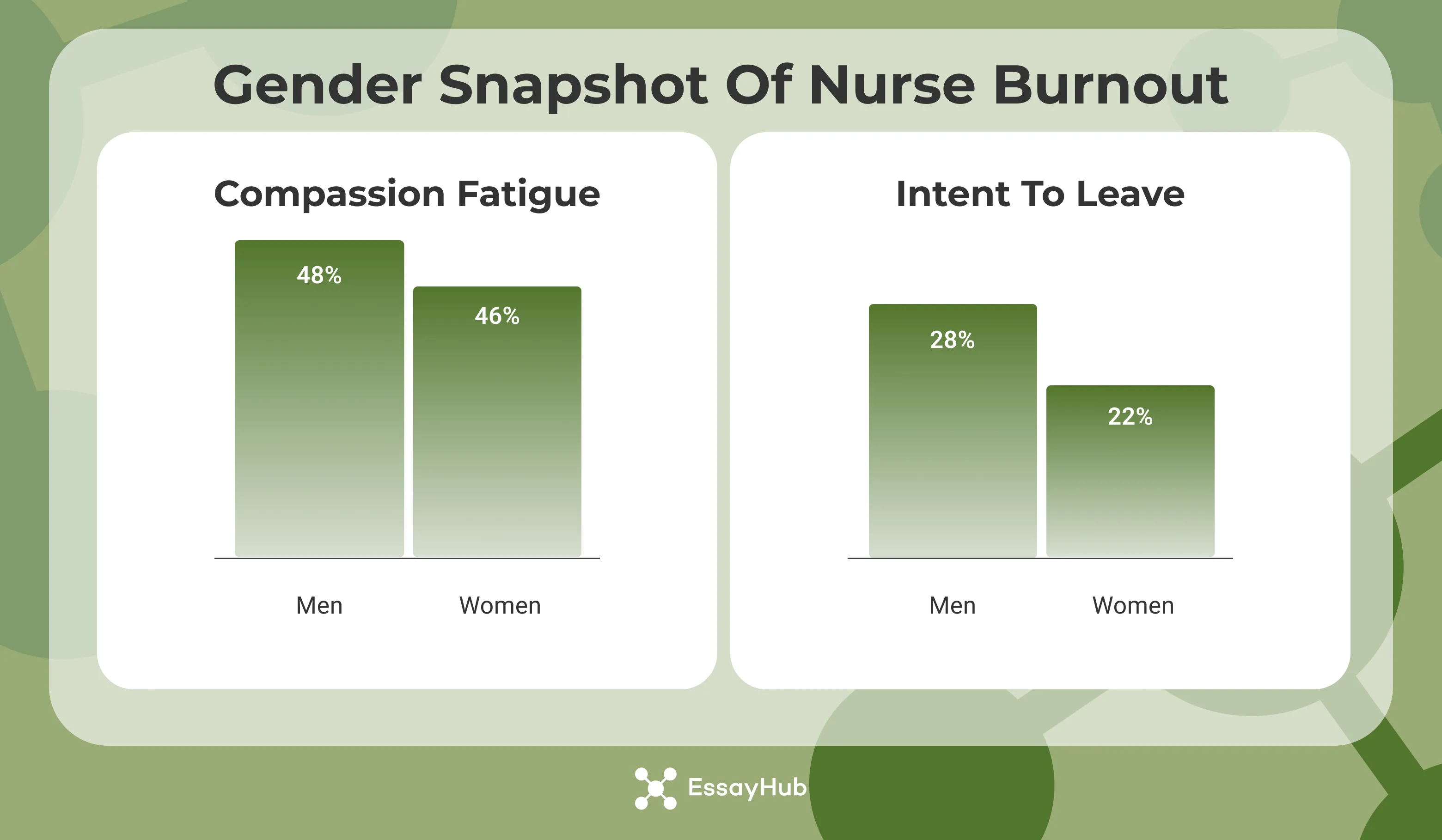
What these statistics on nurse burnout mean for patient care is straightforward. Units lose experience faster when a group with higher exit intent carries critical roles. Managers should track turnover by gender, pair mentorship with early schedule flexibility, and address pay transparency where frustration runs high.
Burnout Statistics by Age
Younger nurses carry a distinct risk.
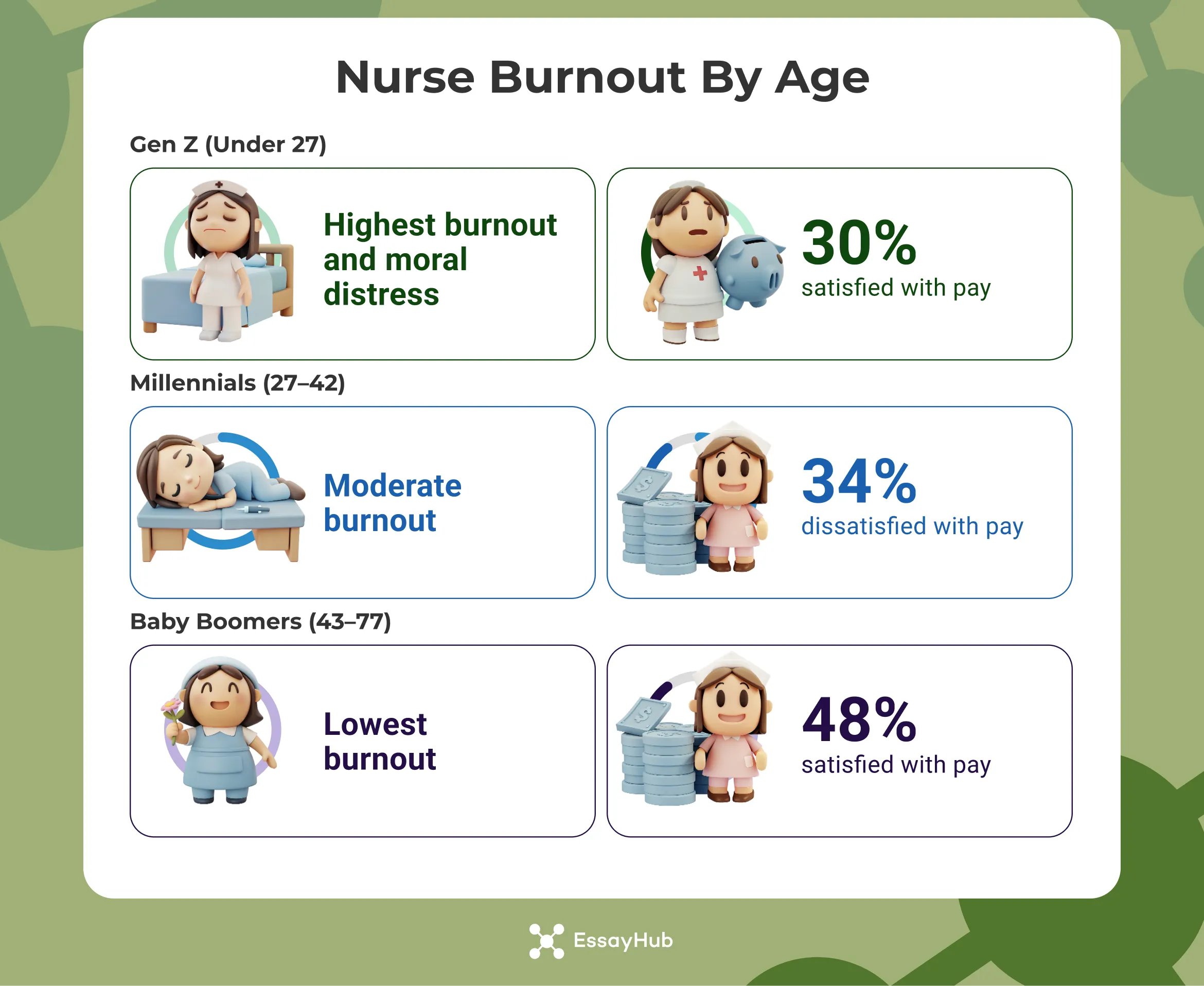
Generation Z nurses (under age 27) report the most burnout, moral distress, and compassion fatigue, which matches what many preceptors notice during orientation blocks. Salary satisfaction shows the divide in hard numbers. About 30 percent of Gen Z report being satisfied with pay. For Baby Boomers (ages 43-77), that figure is near 48 percent. Millennials (ages 27-42) sit between those groups and show the highest share of pay dissatisfaction at roughly 34 percent.
New graduate nurses enter high-acuity environments with less control and thinner recovery windows. Confidence develops slowly while patient acuity stays high. Practical fixes help. Stabilize schedules in the first year, protect sleep, pair new nurses with one consistent mentor, and offer short skill refreshers that target decision fatigue. Each step raises competence and lowers emotional exhaustion.
Burnout Statistics by U.S. Region
Pay and cost of living shape nurse burnout rates in different ways. Average RN salaries cluster near 90 thousand dollars in the West and 88 thousand in the Northeast. The South averages about 77 thousand. The Midwest sits near 75 thousand. Higher pay in coastal regions often comes with high housing costs and persistent staff shortages, which keeps stress high. Lower pay in the South and Midwest stretches household budgets and increases overtime acceptance, which also keeps stress high.
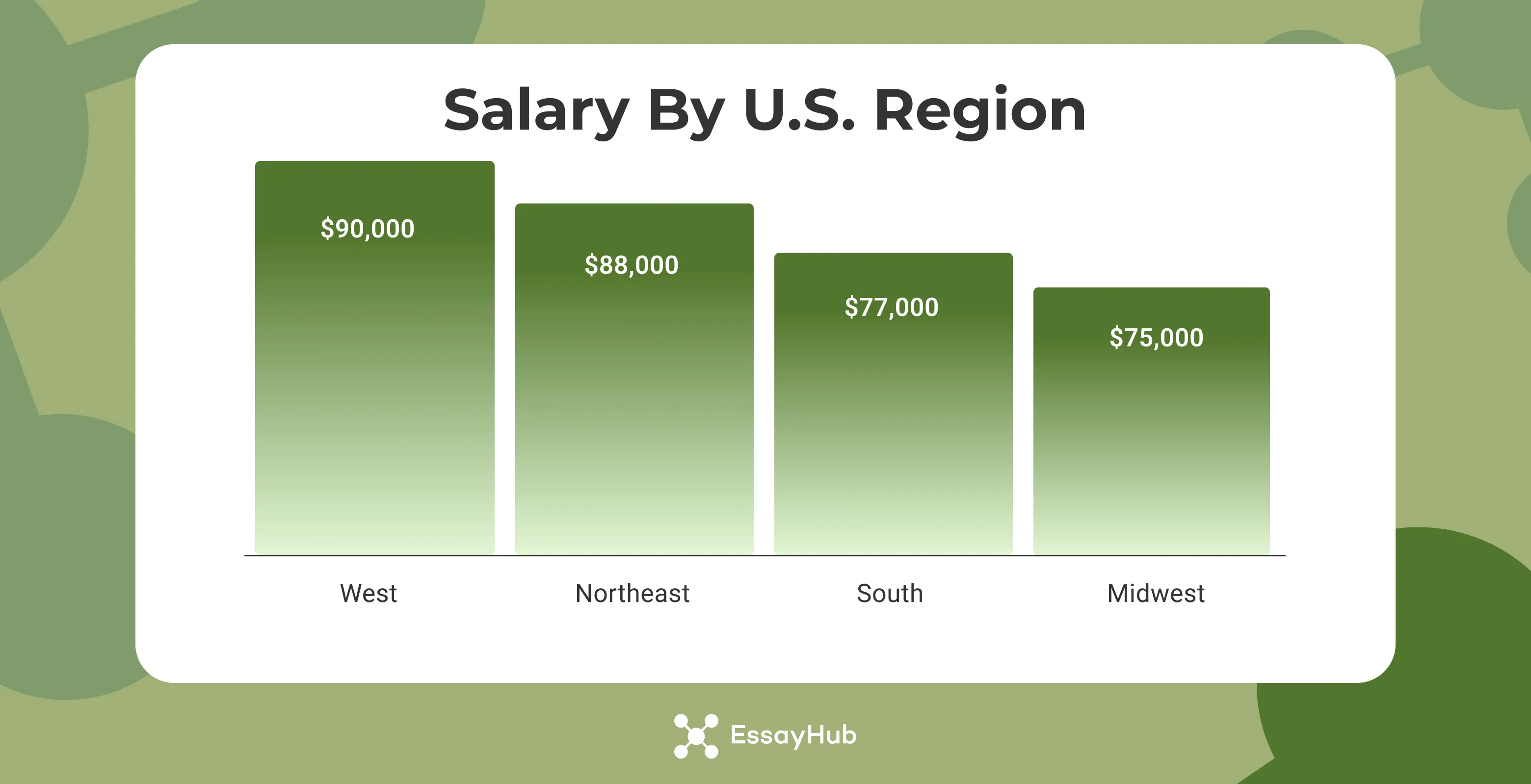
Regional strategy should match the local pinch point. In high-cost areas, protect recovery time and invest in float coverage to offset vacancies. In lower-pay regions, tighten limits on overtime and build retention bonuses that reward experience rather than sheer hours. Across all regions, the goal is the same: lift nurse well being and stabilize patient outcomes by balancing workload, control, and recovery.
Consequences of Nurse Burnout
Burnout does not end with one tired clinician. Burnout results in turnover costs for hospitals, patient safety changes, and drained capacity due to absenteeism and reduced productivity.
- When nurses start planning an exit, the unit already feels it. Nearly a quarter of the workforce is thinking about leaving right now. Registered nurses sit at 23 percent. LPNs and LVNs are close behind at 22 percent.
- A 10% rise in nurses’ intention to leave is associated with a 14% increase in inpatient mortality; adding one patient to a nurse’s workload increases mortality by 3.4%. Burnout is associated with increased medication errors, falls, hospital-acquired infections, and lower patient safety grades and satisfaction, according to a meta-analysis of 85 studies involving 288,581 nurses.
- In a 2024 study, data showed that nurses missed about 13.4% of total working hours due to health problems or psychological distress. Reported losses included an average of 974.8 hours per nurse from absenteeism and 10,630 hours from presenteeism across the sample, highlighting large productivity impacts tied to burnout and poor well-being.
Preventing Nurse Burnout
Burnout eases when three levers move together: demand drops to a humane level, control at the bedside rises, and recovery time becomes non-negotiable. Build nurse burnout prevention across personal habits and team routines.
- Micro-breaks with structure: work in 25-minute focus blocks, then take 5 minutes to stand, sip water, or breathe. Two short cycles during a heavy hour keep accuracy higher than a full hour without a pause.
- Body-doubling on tough stretches: sit with a colleague for charting or med prep. Quiet accountability reduces procrastination and decision fatigue.
- Movement you can keep: ten minutes of hallway laps or a quick stretch before a new admit resets attention better than scrolling a phone.
- Reflective off-ramp: end the shift by writing one clear win and one thing to hand off. Small closure lowers rumination after work.
Team routines that protect energy
- Two-minute huddles at set times: call out patient surges, swap one task each, and name the priority for the next hour. Early redistribution prevents the late-shift crash.
- Buddy checks for breaks: each nurse covers one person’s meal and receives the same in return. Protected breaks actually happen when someone is assigned to make them happen.
A simple two-week reset: ways to prevent nurse burnout
- Week one: run two micro-break cycles per busy hour and use buddy checks for one protected meal each day. Log one moral-distress trigger.
- Week two: add one quiet documentation window per shift and try a two-minute huddle at the top of two hours. Submit the logged trigger for a concrete fix.
Strategies That Reduce Nurse Burnout
The wins come from nurse burnout solutions that lighten the load, programs that restore energy, and schedules that let people recover.
Workplace policies that reduce burnout
Safe staffing rules make the biggest dent. Each added patient per nurse raises burnout odds by about 23 percent and job dissatisfaction by about 15 percent. Units that cut one patient from the average assignment saw burnout drop and inpatient mortality fall by roughly 7 percent.
Mental health support programs
Offer fast access to counseling, peer groups, and brief mindfulness training. Combined programs typically deliver a 20 to 30 percent decline in self-reported burnout within three months, along with better sleep and lower anxiety.
Staffing reforms and flexible scheduling
Cap mandatory overtime, keep reliable float coverage, and use self-scheduling with a few protected requests per nurse. Hospitals adopting these steps report fewer last-minute call-outs, lower absenteeism, and a clear drop in intent to leave.
Final Thoughts
Nurse burnout statistics signal the system’s shortcomings. When demand remains high, control remains low, and recovery time is reduced, patient outcomes decline and costs escalate.
If you’re a nurse trying to stay on top of your assignments while also dealing with everyday stress, EssayHub is the place for you. Reach out to us and ask - write my nursing essay, and let us take the weight off your shoulders.
FAQs
Has Nurse Burnout Increased After COVID-19?
Yes. The pandemic increased acuity, stretched shifts, and heightened infection risk. Many nurses still feel the aftereffects: thinner staffing, heavier assignments, and lingering stress.
Why Is Nurse Burnout a Problem?
Burnout hurts care and teams: medication errors increase when attention slips, patient satisfaction drops when detachment sets in, turnover grows, which drains experience and money. The cycle then feeds itself unless staffing and support improve.
How to Reduce Nurse Burnout?
Lower the load, raise control, and protect recovery. Safe staffing helps first. Flexible scheduling follows. Short, predictable breaks and access to counseling round it out.
How Many Nurses Experience Burnout?
Roughly one-third of nurses report strong burnout symptoms worldwide.
What Is Nurse Burnout?
Nurse burnout is a work-related condition showing itself in emotional exhaustion, detachment from patients, and a fading sense of accomplishment.
- Getie, A., Ayenew, T., Amlak, B. T., Gedfew, M., Edmealem, A., & Kebede, W. M. (2025). Global prevalence and contributing factors of nurse burnout: An umbrella review of systematic review and meta-analysis. BMC Nursing, 24, 596. https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-03266-8
- Lee, Y.-L., Dai, J.-W., Li, X.-W., Chiang, M.-Y., Chen, P.-T., Lin, Y.-C., & Wang, C.-H. (2024). Prevalence and the associated factors of burnout among the critical healthcare professionals during the post-pandemic era: A multi-institutional survey in Taiwan with a systematic review of the Asian literatures. BMC Public Health, 24, 3480. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-21084-6
- Meeker, Z. (2025, April 28). 2024 nurse burnout statistics: A detailed look. https://www.nurse.com/blog/2024-nurse-burnout-statistics-a-detailed-look/
- SE Healthcare. (2025, February 20). New global study confirms nurse burnout crisis—Patient safety and healthcare sustainability at risk. https://sehealthcaresolutions.com/news/new-global-study-confirms-nurse-burnout-crisis-patient-safety-and-healthcare-sustainability-at-risk
- SE Healthcare. (2024). The state of nurse burnout in 2024 [White paper]. https://45389480.fs1.hubspotusercontent-na1.net/hubfs/45389480/PDFs/SEHQC-WhitePaper-Burnout2024-12.24.2.pdf






